Endobronchial ultrasound (EBUS) procedures have dramatically transformed the landscape of respiratory care, particularly in the field of interventional pulmonology. EBUS provides minimally invasive access to lungs and surrounding lymph nodes, offering a safer and more efficient alternative to conventional diagnostic procedures like mediastinoscopy.
But while EBUS advances patient care, it also introduces new complexities in the realm of medical coding and billing, with numerous codes describing various aspects of the procedure. Accurate coding of EBUS procedures is not merely a matter of administrative detail, but an essential element in the effective management of healthcare systems.
Proper assignment of Current Procedural Terminology (CPT) codes ensures that the intricacies of the performed procedures are well-documented, leading to fair reimbursement for healthcare providers and transparency for patients. CPT codes also serve as a universal language among healthcare providers, coders, billers, insurance companies, and other relevant stakeholders.
They provide an efficient way to convey crucial information about medical services and procedures. With a proper understanding of EBUS CPT codes, healthcare providers can better navigate the labyrinth of medical billing, reducing errors and optimizing revenue cycle management.
EBUS Procedures
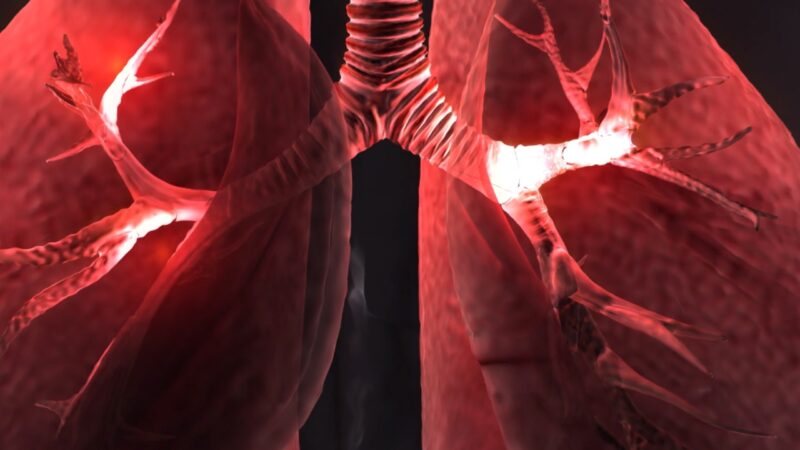
EBUS procedures represent a revolutionary advancement in diagnosing and staging lung cancer, among other respiratory conditions. These procedures leverage a flexible bronchoscope equipped with ultrasound capabilities, providing real-time imaging that enables doctors to see beyond the walls of the airways and into surrounding tissues and organs, including lymph nodes.
Among the most significant advantages of EBUS procedures is their minimally invasive nature, which reduces risks and recovery time for patients. They also provide a high degree of accuracy, enabling targeted sampling of lung tissue and lymph nodes. This accuracy makes Endobronchial ultrasound a critical tool for diagnosing lung cancer and other conditions, and for staging lung cancer to guide appropriate treatment plans.
However, with the advantages of EBUS come complexities in procedural coding. There are several distinct Endobronchial ultrasound procedures, each with its own associated CPT codes, and further codes for associated actions such as biopsy or lymph node sampling. Understanding and correctly applying these codes is crucial to accurately reflecting the services provided.
Common EBUS CPT Codes
These procedures encompass various tasks, including but not limited to bronchoscopic guidance, needle aspiration, biopsy, and lymph node sampling, each with its own CPT code. For instance, 31652 is the CPT code for bronchoscopy, EBUS guidance, and sampling of mediastinal and/or hilar lymph nodes via transbronchial needle aspiration (TBNA).
In the realm of biopsy, CPT code 31653 covers bronchoscopy with EBUS guidance and biopsy of lung or mediastinum via transbronchial needle aspiration (TBNA), whereas 31654 is for bronchoscopy with EBUS guidance and transbronchial lung biopsy. Understanding these codes is crucial as different aspects of these procedures have distinct codes, and failing to apply them correctly can result in denied claims or loss of revenue.
These codes also paint a vivid picture of the specific services provided, leading to a greater understanding of the procedure among all stakeholders. Proper application of these codes not only ensures fair reimbursement but also enhances transparency and trust between healthcare providers, insurance companies, and patients.
Coding Guidelines and Documentation Requirements

Coding guidelines provide a roadmap for the effective and accurate assignment of CPT codes. They ensure consistency across the coding process, aiding in minimizing coding errors and discrepancies that could lead to claim denials or underpayments. For EBUS procedures, understanding and adhering to the specific coding guidelines is of paramount importance. The quality of documentation also plays a significant role in the coding process.
Detailed and accurate documentation can help coders assign the most appropriate codes for EBUS procedures. Such documentation should include thorough patient history, the reasons for performing the procedure, a detailed report of the procedure itself, and the outcomes or findings from the procedure.
Remember, inadequate documentation is a common reason for claim denials. Therefore, healthcare providers must ensure their documentation supports the assigned CPT codes, providing a clear picture of the services rendered. This aids in the audit process, prevents coding errors, and helps optimize the reimbursement process.
Challenges and Pitfalls in EBUS Coding
Coding for EBUS procedures is fraught with challenges and potential pitfalls. The procedures are complex, and there are numerous codes to choose from, creating ample room for error. Mistakes in coding can lead to substantial financial losses and damage the reputation of healthcare providers. One common pitfall is over-coding or under-coding, which happens when coders assign a code that doesn’t accurately reflect the services provided.
Over-coding can lead to overbilling, which is illegal and can result in fines, penalties, and loss of trust among patients and insurers. Undercoding, on the other hand, may lead to a loss of deserved revenue. To avoid these errors, it’s essential for coders to have a thorough understanding of EBUS procedures and associated CPT codes. This includes a detailed understanding of the procedure notes, the proper application of modifiers, and the latest changes and updates in the coding guidelines.
Updates and Changes
The realm of medical coding, including these codes, is not static. It evolves over time to reflect the advancements in medical technology and procedures. Keeping abreast of the latest updates and changes in EBUS coding is crucial for healthcare providers to maintain compliance and accuracy in their billing process. For instance, in the recent past, there have been significant changes in the way EBUS procedures are coded.
The AMA revised the bronchoscopy CPT codes, including the EBUS codes, which now include a series of bundled codes. These revisions are intended to reduce confusion and the burden of coding, providing a simpler and more streamlined approach to EBUS coding. These changes have significant implications for coding practices. Healthcare providers must understand these revisions and adjust their coding and billing practices accordingly to avoid claim denials and ensure they’re fairly compensated for their services.
Cardiopulmonary stress tests, commonly referred to by their CPT codes, play a pivotal role in the diagnosis and assessment of cardiovascular and respiratory conditions.
Resources and Tools
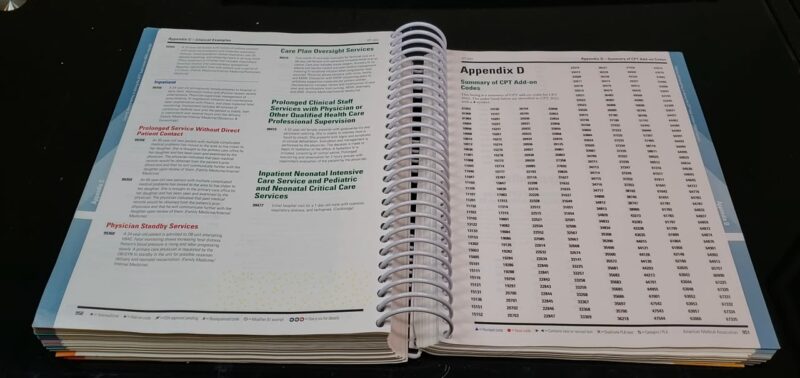
Navigating the intricate landscape of these codes can be challenging. However, several resources and tools can help simplify this process, ranging from coding manuals to online references and software tools. The AMA’s CPT Professional Edition is an invaluable resource that provides detailed explanations of all CPT codes, including those for EBUS procedures.
Online platforms like the AMA’s CPT Assistant and the Centers for Medicare & Medicaid Services (CMS) also provide updated information on coding changes and best practices. In addition, specialized medical coding software can aid in the coding process, providing a searchable database of CPT codes and updates, automated code verification, and other tools to minimize coding errors and streamline the billing process.
Training and Education
Due to the complexity and importance of EBUS coding, specialized training, and education is essential for healthcare providers and coders. Courses, workshops, and certifications can provide the necessary knowledge and skills to accurately code EBUS procedures and navigate the evolving landscape of medical coding. Several organizations offer coding education, including the American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA).
Both offer certification programs that demonstrate proficiency in medical coding, including CPT coding for complex procedures like EBUS. Continuing education is also crucial as it allows coders to stay updated on changes in coding rules and regulations, technological advancements, and evolving best practices. Therefore, investing in training and education can pay off by reducing coding errors, improving reimbursement rates, and enhancing the overall efficiency of the billing process.
Collaborating with Billing Professionals

Working with experienced billing professionals can be highly beneficial for it. These professionals have a deep understanding of the medical coding system, including the specific codes for EBUS procedures, and are adept at navigating the complex rules and regulations of medical billing. Collaborating with billing professionals can help streamline the coding process, reduce errors, and optimize reimbursement rates.
They can help identify coding errors or discrepancies, ensure compliance with coding guidelines and regulatory requirements, and handle any issues or inquiries from insurance companies or patients. Moreover, the collaboration between healthcare providers and billing professionals allows for a more efficient and effective billing process, freeing providers to focus more on patient care and less on administrative tasks.
This collaborative approach can lead to better patient outcomes, higher reimbursement rates, and improved financial health for healthcare providers.
Conclusion
In the realm of respiratory care, EBUS procedures have emerged as a game-changer. However, these innovative procedures come with a unique set of coding challenges. A thorough understanding of EBUS CPT codes, adherence to coding guidelines, detailed documentation, and continuing education are essential for accurate coding and optimal reimbursement.
Moreover, staying updated on changes in EBUS coding, leveraging useful resources and tools, and collaborating with billing professionals can significantly simplify the coding process. With a comprehensive approach to EBUS coding, healthcare providers can ensure they’re fairly compensated for their services while maintaining transparency and trust among all stakeholders. In essence, accurate EBUS coding serves as a bridge that connects healthcare innovation with sustainable healthcare provision.

