Ventilator-associated pneumonia (VAP) represents a crucial concern in intensive care units (ICUs) worldwide, posing substantial threats to patient safety. It’s not only associated with increased morbidity and mortality, but it also significantly inflates healthcare costs and prolongs hospital stays. This article aims to illuminate essential strategies for navigating VAP guidelines, presenting an actionable roadmap for healthcare professionals to bolster infection prevention and control.
VAP prevention can be a complex topic, involving various strategies, techniques, and guidelines. However, by breaking it down into its key components, we can better understand the tools we have at our disposal and implement them more effectively. This understanding is critical not just for ICU physicians and nurses, but for all healthcare professionals. Everyone plays a role in preventing VAP and enhancing patient outcomes.
The importance of this topic cannot be overstated, and so the goal of this article is to provide a comprehensive guide to VAP prevention. We’ll discuss risk factors, prevention strategies, ventilator management best practices, the role of antibiotic stewardship, and more. It’s a guide tailored to a diverse readership, turning the complexity of the subject into easily digestible insights for everyone.
VAP Guidelines
VAP prevention guidelines provide evidence-based strategies that help healthcare teams minimize the risk of VAP. These guidelines, developed by various organizations like the Centers for Disease Control and Prevention (CDC) and the American Thoracic Society (ATS), offer a structured approach to VAP prevention and control. These guidelines are created by panels of experts who review the latest research and translate the findings into practical, step-by-step recommendations.
They cover a broad spectrum of areas, from patient positioning and oral care to ventilator maintenance and antibiotic stewardship. The goal is to provide healthcare professionals with a comprehensive toolkit to reduce VAP incidence. Adherence to these guidelines is crucial, and each recommendation plays a vital role in preventing VAP.
It’s not just about knowing these guidelines but also understanding them – appreciating the ‘why’ behind each recommendation. That’s where we’ll focus next, breaking down these guidelines into actionable strategies and explaining why each one matters.
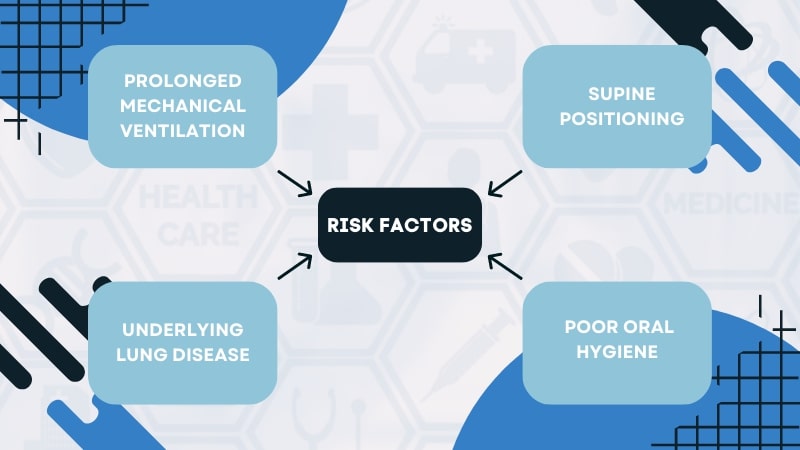
Risk Factors and Identification
Understanding the risk factors for VAP is critical to its prevention. Some of the known risk factors include prolonged mechanical ventilation, supine positioning, underlying lung disease, and poor oral hygiene. By identifying and managing these risks, we can proactively reduce the chance of VAP occurrence. Clinical signs of VAP include worsening oxygenation, fever, purulent tracheal secretions, and new or progressive radiographic infiltrates.
However, VAP diagnosis can be challenging due to the non-specific nature of these signs. Therefore, a combination of clinical, radiological, and microbiological criteria is often used to improve diagnostic accuracy. Identification is only the first step; understanding the risk factors and signs enables us to take preventive measures. Once identified, we can strategize and apply the guidelines to mitigate these risks, ultimately improving patient care and outcomes.
Strategies for Infection Prevention
Preventing it involves multiple strategies, including hand hygiene, adhering to bundle protocols, oral care, and maintaining a sterile environment. Hand hygiene is perhaps the most straightforward and cost-effective measure. By properly washing and sanitizing hands before and after patient contact, healthcare workers can significantly reduce the risk of cross-contamination.
Bundle protocols involve a set of evidence-based interventions for patients with mechanical ventilation. These may include elevation of the head of the bed, daily sedation breaks, and peptic ulcer disease prophylaxis, among others. Adherence to these protocols has been shown to reduce VAP incidence significantly.
Oral care, particularly with chlorhexidine, can significantly reduce the incidence of VAP by decreasing the colonization of pathogenic bacteria in the mouth. Similarly, maintaining a sterile environment and handling equipment properly also play a crucial role in preventing it. It’s about cultivating a culture of safety where every action taken aims to reduce infection risk.
Ventilator Management and Best Practices
Proper ventilator management is vital in reducing VAP risk. Strategies include minimal sedation, early mobilization, and using endotracheal tubes with subglottic suctioning. Each of these strategies addresses a specific risk factor associated with mechanical ventilation. Sedation management aims to reduce the duration of mechanical ventilation. The longer a patient remains on a ventilator, the higher the risk of VAP.
Therefore, strategies such as daily sedation breaks and utilization of a sedation protocol can promote earlier liberation from mechanical ventilation. Subglottic suctioning helps prevent the microaspiration of contaminated secretions that pool above the cuff of the endotracheal tube.
Tubes with continuous subglottic suctioning capabilities should be used for patients expected to be on mechanical ventilation for more than 48 hours. Ventilator management isn’t just about the mechanics of ventilation, but about managing the whole patient and the environment around them.
Role of Antibiotic Stewardship
Inappropriate use of antibiotics can lead to antibiotic resistance and increase VAP risk. Thus, antibiotic stewardship — the optimal selection, dose, and duration of antibiotic therapy — plays a pivotal role in VAP prevention. It’s about using antibiotics judiciously and responsibly to preserve their effectiveness.
A well-structured antibiotic stewardship program helps promote the appropriate use of antibiotics, improve patient outcomes, reduce microbial resistance, and decrease unnecessary costs. Strategies may include prospective audit and feedback, guideline implementation, and de-escalation of therapy when appropriate. Furthermore, empiric antibiotic therapy should be based on local microbiologic data and adjusted according to culture results.
Prompt discontinuation of antibiotics once the bacterial infection is ruled out is also essential to prevent resistance. It’s about achieving a balance – treating infections effectively while preventing the emergence of antibiotic resistance.
Education and Training
Education is the cornerstone of any successful infection control initiative, including VAP prevention. Healthcare professionals need to understand the importance of VAP prevention, the risk factors involved, and the steps they can take to prevent VAP. Various training programs and resources are available to assist healthcare staff in gaining these insights.
From online courses and webinars to hands-on training and workshops, there are numerous opportunities for healthcare professionals to learn and grow. Such programs not only impart knowledge but also inspire a commitment to patient safety and quality improvement. Healthcare professionals are life-long learners, and the more we learn, the better we become at preventing it. Effective education and training programs can instill the skills and knowledge required to make this happen.
Surveillance and Data Collection
Surveillance and data collection play a crucial role in monitoring VAP rates and identifying trends. By regularly collecting and analyzing data, healthcare teams can identify areas for improvement and track the impact of their prevention efforts. Tools like the National Healthcare Safety Network (NHSN) provide standardized methodologies for data collection and reporting.
Using these tools, healthcare teams can collect reliable data, compare their performance with national benchmarks, and develop strategies for improvement. Surveillance isn’t just about collecting data; it’s about understanding what the data means and using it to drive quality improvement. By tracking our performance and striving for continuous improvement, we can make significant strides in preventing VAP.
Collaboration and Interdisciplinary Approach
VAP prevention requires collaboration among healthcare teams. It’s not the responsibility of a single individual or department but a collective effort. By working together, sharing insights, and supporting each other, we can effectively implement VAP prevention strategies. Interdisciplinary communication and teamwork are critical to this process.
From physicians and nurses to respiratory therapists and infection control practitioners, everyone plays a vital role. Regular meetings, briefings, and debriefings can help foster this collaborative culture. By fostering a culture of collaboration, we can break down silos and work towards a common goal – preventing VAP and improving patient outcomes. This team-based approach is the cornerstone of effective VAP prevention.
Quality Improvement Initiatives
Quality improvement initiatives for VAP prevention and control are an integral part of healthcare delivery. These initiatives use performance indicators and benchmarks to measure success and drive continuous improvement. Performance indicators, such as VAP rates, adherence to prevention measures, and patient outcomes, provide objective measures of success.
By tracking these indicators, we can identify areas for improvement and evaluate the impact of our interventions. Benchmarks, on the other hand, provide a standard of excellence against which we can compare our performance. They inspire us to strive for continuous improvement and achieve the highest standards of care. Quality improvement isn’t a destination but a journey, a constant pursuit of excellence in patient care.
Challenges and Future Directions
While we have made significant strides in VAP prevention, challenges remain. These include sustaining prevention efforts, overcoming resource limitations, and navigating the complexities of healthcare systems. Yet, each challenge presents an opportunity for learning and improvement. Future directions in VAP prevention research and guidelines include further refining diagnostic criteria, exploring new prevention strategies, and leveraging technology to enhance care delivery.
As we look to the future, it’s about embracing innovation, learning from our experiences, and continually striving to improve. By acknowledging these challenges and exploring future directions, we can drive progress in VAP prevention and control. It’s about turning challenges into opportunities and driving the evolution of patient care.
Conclusion
Preventing VAP is a vital task that requires understanding, commitment, and collaboration. By understanding VAP and its impact, adhering to established guidelines, implementing preventive measures, and promoting antibiotic stewardship, we can make a significant impact.
While the journey toward VAP prevention can be challenging, it’s a journey worth undertaking. Not just for the cost savings, but for the lives we can save, the suffering we can prevent, and the quality of care we can enhance. In the end, it’s about delivering the highest quality of care for our patients – and that’s a mission we can all get behind.